Researcher opens behavioral health clinic
Gabrielle Plucknette-DeVito
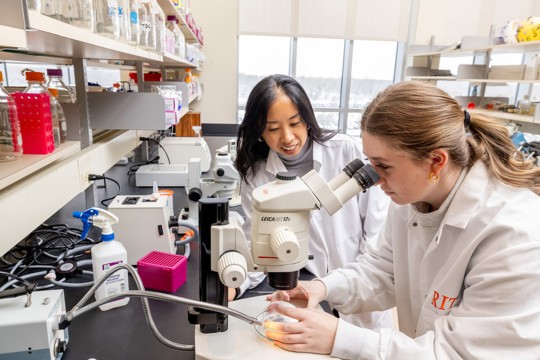
Caroline Easton, professor of biomedical sciences, opened a behavioral health clinic on campus last fall. She sees the clinic as a community resource.
RIT’s behavioral health program is expanding in new directions with a clinic on campus and federal funding to deliver addiction treatment in rural communities in upstate New York and New Hampshire.
These partnerships and services create momentum for the Priority Behavioral Health & Clinical Psychology Internship led by Caroline Easton ’90 (biotechnology), professor of biomedical sciences.
The program was funded in 2018 by the U.S. Department of Health and Human Services’ Health Resources and Services Administration to fill a shortage of mental health professionals, especially with addiction expertise, in the Rochester area.
The RIT Priority Behavioral Health clinic gives therapy interns experience conducting in-person and telehealth sessions and assessment services under the supervision of licensed clinical psychologists. The training clinic is open to anyone at RIT and in the wider community, and services are free of charge.
The clinicians practice cognitive behavioral therapy, motivational enhancement therapy, and mindfulness skills, as well as behavioral health screenings and consultations, psychological testing, digital therapies, and tele-behavioral health.
Easton sees the clinic as a resource for the community, especially for people who have lost their jobs during the COVID-19 pandemic and who may not have health insurance or money for co-pays. “The clinic is not only for people struggling with addiction, anxiety, and depression,” she said. “Right now, people are dealing with grief and loss, social isolation, and health anxiety. We will take clients who just need somebody to talk to.”
RIT behavioral health researchers in the biomedical sciences program—Easton; Cory Crane, associate professor; and Cassandra Berbary, visiting assistant professor—won additional funding from the Health Resources and Services Administration to deliver mental health and addiction treatment to underserved populations.
The federal agency is supporting a $1.4 million telehealth program for homeless residents at the House of Mercy shelter, which was deployed during the New York state shutdown, and more recently, a $1 million telehealth outreach for rural and underserved communities in New York and in New Hampshire, addressing opioid addiction and other forms of substance abuse.
Residents of New York’s Genesee County, Wyoming County, and Cayuga County and New Hampshire’s Grafton County may be eligible for the program. The participating clinical sites were selected through RIT’s strategic alliance with Rochester Regional Health and a new partnership with Ammonoosuc Community Health Services in New Hampshire, facilitated by the CEO and RIT alumnus Ed Shanshala II ’00 MS (health systems management).
“Our telehealth training program is especially relevant during the pandemic and the new risk factors it has created for rural residents with addiction issues and for their families,” she said. “The pandemic has led to unemployment, loss of health insurance, opioid/substance relapse, anxiety and depression, grief, and personal loss.”
Easton’s research connects the dots between intimate partner/domestic violence, mental health, and substance abuse. Her Substance Abuse-Domestic Violence Behavioral Model reduces clients’ drug and alcohol use while teaching coping skills for handling negative emotions. Grounded in cognitive behavioral therapy, the client-centered approach has measurable outcomes proven in randomized control trials funded by the Donaghue Foundation and the National Institute of Drug Abuse.