Rochester Psychology Internship Consortium
- RIT/
- College of Health Sciences and Technology/
- Academics/
- Rochester Psychology Internship Consortium
- Competencies
- Accreditation
- Structure of the Program
- Internship Positions
- Evidence-Based Practices
- Research and Scholarship
- Supervision
- Training Faculty
- Didactic Seminar Series
- Stipend, Benefits, and Resources
- Application Process and Selection Criteria
- Internship Handbook
- Intern Expectations
- HRSA Grant Funding
- Internship Admissions, Support, and Initial Placement Data
- Past Intern Cohorts
- Diversity Resources
Overview
Rochester Psychology Internship Consortium at RIT represents a cooperative endeavor between RIT’s College of Health Science and Technology and clinical placement sites within Rochester Regional Health, Hillside Children’s Center, Coordinated Care Services Inc (CCSI), Rochester Psychological Assessment & Testing (RPAT), Ontario County Mental Health (OCMH), and University of Rochester Medical Center (URMC) Strong Recovery. Rochester Institute of Technology’s College of Health Science and Technology functions as a hub for the internship faculty, didactic training, and administrative processes.
This internship year is first and foremost a supervised, intensive, experiential learning opportunity focused on the delivery of psychological services. The program embraces a scientist-practitioner model in which theory and evidence routinely inform professional practice and each intern has protected time to pursue a scholarly activity that can center on research, program evaluation, clinical care, or education. The training is competency-based. Each intern will have a year-long primary placement at one of the clinical sites. While in their primary clinical settings, interns provide supervised behavioral health intervention and assessment services to individuals from diverse backgrounds. Intervention may include individual, group, and/or family therapy, and may be provided for children, adolescents and/or adults, depending on the primary clinical placement. Psychological assessment is also provided at each placement site, and interns are expected to administer, interpret, and provide written synthesis of psychological test batteries. Therapy clients, number of assessments, consultation work, and research vary depending on the specific site. Interns across clinical sites have the opportunity to gain experience working with and consulting across a variety of disciplines as a major component of their training program, as each primary placement involves collaboration across various systems of care. Experiences may involve collaboration and consultation with various agencies and/or providers within multiple care disciplines and settings.
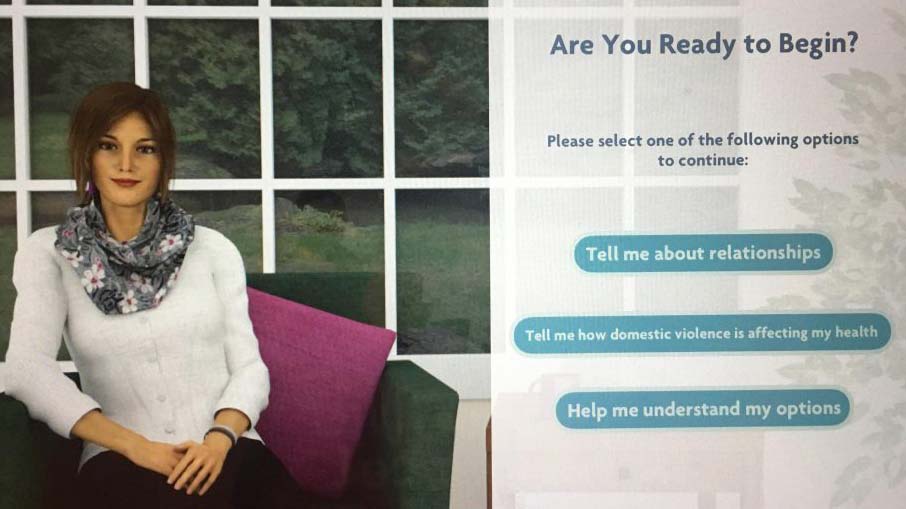
Our training and education program is dedicated to developing the next generation of leaders in the field using innovative and advanced technologies (e.g, Telehealth and Technology Assisted Interactive Tools for Clients), which is a core mission and trademark of RIT. All interns are provided with didactic and experiential training in the use of telehealth and interactive therapeutic technologies. Specifically, all interns are provided with the opportunity to engage in both in-person and telehealth treatment with homeless clients.
All interns are expected to conduct research at the internship sites through at least one ongoing scholar project, the focus of which is determined collaboratively between the primary supervisors and the intern. For more information on possible research areas please visit: Favtech | RIT
A priority is placed on professional development, including assistance to doctoral fellows in securing opportunities after internship such as post-doctoral fellowships and employment. Our clinical sites have an interest in hiring the next generation of leaders.
For additional details regarding internship program, please consult the Priority Behavioral Health Internship Handbook.
Check out these possible opportunities available during your internship
Rochester Institute of Technology Intersections:
The RIT Podcast Ep. 29: The Benefits of Telehealth!
Competencies
Internship Program competencies are as follows:
Competency 1: Interns will achieve an intermediate to advanced level of competence in Evidence-Based Intervention
Competency 2: Interns will achieve an intermediate to advanced level of competence in Evidence-Based Assessment
Competency 3: Interns will achieve an intermediate to advanced level of competence in Ethical and Legal Standards
Competency 4: Interns will achieve an intermediate to advanced level of competence in Cultural and Individual Diversity
Competency 5: Interns will achieve an intermediate to advanced level of competence in Research
Competency 6: Interns will achieve an intermediate to advanced level of competence in Professional Values, Attitudes, and Behaviors
Competency 7: Interns will achieve an intermediate to advanced level of competence in Interprofessional and Interdisciplinary Consultation
Competency 8: Interns will achieve an intermediate to advanced level of competence in Supervision
Competency 9: Interns will achieve an intermediate to advanced level of competence in Communication and Interpersonal Skills
Competency 10: Interns will achieve an intermediate to advanced level of competence in Telehealth and Interactive Therapeutic Technologies
Competency 11: Interns will achieve an intermediate to advanced level of competence in Clinical Leadership and Career Development within Ambulatory Behavioral Health Settings
Accreditation
APPIC: Our program is a member of APPIC.
APA: Our program is APA accredited.
Questions related to the program’s accreditation status should be directed to the Commission on Accreditation:
Office of Program Consultation and Accreditation
American Psychological Association
750 1st Street, NE, Washington, DC 20002
Phone: 202-336-5979
Email: apaaccred@apa.org
APPIC Membership Status
Structure of the Program
The internship begins on July 1st, concludes on June 30th of each academic year, and provides 2000 hours of training. Interns in this program are referred to as "psychology interns." Interns will complete the internship program over 12 months on a full-time (40 hours/week) basis. Interns are matched to one of the following clinical tracks; Coordinated Care Services Inc (CCSI), Hillside Children’s Center, Rochester Addiction-Forensic Clinical Research at Strong Recovery, Rochester Neuroscience, Pain, and Spinal Care, Rochester Regional Health (RRH) Outpatient Behavioral Health (Adult), Rochester Regional Health (RRH) Outpatient Behavioral Health (Child/Adolescent), Rochester Regional Health (RRH) Integrated Care, Rochester Regional Health (RRH) Neuropsychology at the Neuroscience Institute, Rochester Psychological Assessment & Testing (RPAT), or Ontario County Mental Health (OCMH).
Interns spend 4 days a week with their clinical track and 1 day a week at Rochester Institute of Technology’s main campus for additional supervision, didactics, clinical discussions, and scholar activities.
The training curriculum has been designed in accordance with the internship program’s required competencies. Each competency is met through both experiential and didactic training. While in their primary clinical settings, interns provide supervised behavioral health intervention and/or assessment services to individuals from diverse backgrounds. Intervention may include individual, group, and/or family therapy, and may be provided for children, adolescents and/or adults, depending on the primary clinical placement. Psychological assessment also is provided at each placement site, and interns are expected to administer, interpret, and provide written synthesis of psychological test batteries. Therapy clients, number of assessments, consultation work, and research vary depending on the specific site.
Interns across clinical sites have the opportunity to gain experience working with and consulting across a variety of disciplines as a major component of their training program, as each track involves collaboration across various systems of care. Experiences may involve collaboration and consultation with various agencies and/or providers within multiple care disciplines and settings.
All interns are provided with didactic and experiential training in the use of telehealth and interactive therapeutic technologies, as these skills are critical for providers in highly underserved areas and are core to the mission of the Rochester Institute of Technology.
Interns are provided with regular supervision, which focuses on clinical skills development as well as addressing such issues as ethics, diversity, and professionalism. Interns are also provided with training in the effective provision of supervision and are given opportunities to practice these skills through the provision of supervision to undergraduate students who provide support to the interns’ scholar projects. All training goal areas are additionally supported through the provision of relevant didactics provided by content experts.
All Interns are expected to conduct research at the internship sites through at least one ongoing “scholar project”, the focus of which is determined collaboratively between the primary supervisors and the intern.
Internship Positions
Interns are matched to one of the following clinical tracks; Coordinated Care Services Inc (CCSI), Hillside Children’s Center, Rochester Addition-Forensic Clinical Research at Strong Recovery, Rochester Regional Health (RRH) Outpatient Behavioral Health (Adult), Rochester Regional Health (RRH) Outpatient Behavioral Health (Child/Adolescent), Rochester Regional Health (RRH) Integrated Care, Rochester Regional Health (RRH) Neuropsychology at the Neuroscience Institute, Rochester Psychological Assessment & Testing (RPAT), or Ontario County Mental Health (OCMH).
Coordinated Care Services, Incorporated (CCSI), provides a broad array of consulting services specifically tailored to meet the needs of behavioral and physical healthcare providers, social and human service departments, state agencies, school districts and community-based organization in Monroe County, across New York State, and beyond. CCSI’s Consulting Services includes practice transformation (trauma-responsive care, DEI), strategic analytics, quality improvement, fiscal practice improvement and digital solutions and technology.
The CCSI Clinical Track would provide trainees with opportunities to develop skills in systems level intervention and transformation with the general goals of increasing access to high quality healthcare services for underserved and marginalized populations, improving lives, and strengthening communities. CCSI consults with a broad array of sectors including organizations in behavioral, mental, and physical health, community-based organizations, education (K-12 and higher education), faith-based organizations, and government agencies. Project scopes range from one-time engagements to multiple year initiatives. Interns function as a member of project teams and activities may include conducting literature reviews, focus groups, identifying and measuring outcomes, supporting adoption of equity-focused, trauma responsive practices, creating informative and action-oriented reports for agencies and communities, and presenting information on topics of interest to organizations. Over the course of the year, interns will have the opportunity to participate on multiple project teams which are informed by areas of interest. Interns will obtain specific experience supporting trauma-responsive practice and diversity, equity, and inclusion initiatives. This track will also allow interns to have access to a number of datasets at CCSI from which to develop a scholar project that is of interest to both CCSI and the intern (Medicaid claims data for NYS, Adverse Childhood Experiences, Youth Risk Behavior Survey, as well as impact of state dollars on system transformation efforts).
Hillside Children’s Center is a non-profit organization consisting of more than 100 coordinated programs in 41 locations across New York and Maryland which provide comprehensive health, education, and human services for children and families. The placements are located at one of Hillside Children’s Center residential treatment center in and around Rochester, NY. Interns at this placement site work as part of a multidisciplinary team treating youth placed in residential care from across New York State. The intern is responsible for psychological evaluations, consultation with the treatment team including family and external funders, and delivery of evidence-based group and individual therapy. Interns placed with the Hillside Children’s Center will work directly with youth and families who have experienced complex and intergenerational trauma. Evidence practices used include dialectical behavior therapy and trauma-focused cognitive behavioral therapy.
Interns in the University of Rochester Medical Center (URMC)'s Addiction Forensic Clinical Research at Strong Recovery Track will focus their time on developing expertise in translational clinical research. Interns are integrated into a multidisciplinary team of providers, collaborating closely with psychiatrists, substance use counselors, psychologists, and other clinicians. Interns have the opportunity to conduct both individual and group therapy with clients experiencing co-occurring substance use and mental health disorders. Interns conduct psychological and neurocognitive testing to aid in diagnostic clarity and help shape treatment plans tailored to the needs of each client. Clinical activities utilize advanced interactive healthcare technologies to provide evidence based behavioral health care. Interactive technologies include digital assessments and behavior tracking tools, interactive digital health care intervention platforms (e.g., a User Friendly, Customizable Avatar Assisted CBT Platform [RITch®CBT], 3D Organ Simulation Tools for Motivational Interviewing, Virtual Reality Mindfulness Tools). Under the supervision of a licensed clinical psychologist, interns may complete court-ordered competency to stand trial assessments and mental health evaluations (e.g., Mental Health and Drug Court Evaluations).
The internship offers both didactic and supervisory experiences focused on the etiology of substance use and violent behavior within the context of empirically supported interventions. Research activities also include using the digital tools with wearable biosensor research, biomarker research, and tele-health services. Interns will make meaningful contributions to ongoing research projects, including developing and submitting manuscripts for publication using existing data sets, assisting with federally funded randomized controlled trials evaluating treatments for comorbid substance use disorders and aggression, and analyzing dyadic data from couples in alcohol manipulation studies, as well as EMA data exploring the proximal relationships between substance use and aggression.
The RRH Adult track will provide trainees with opportunities at outpatient mental health clinics including RRH’s Evelyn Brandon Health Clinic, Greece Mental Health Clinic, and Genesee Mental Health Clinic. Four interns are placed within clinics treating adult (18+) clients. The psychiatric characteristics of clients treated includes the full diagnostic range of the DSM-5. Interns across clinics have the opportunity to conduct individual therapy, family therapy, and group therapy. Interns will also engage in psychological assessment in order to provide differential diagnoses and recommendations for ongoing treatment/referrals. Interns will learn efficient evaluation and report writing procedures. Interns at RRH work closely with a multi-disciplinary team of licensed social workers, licensed mental health counselors, substance abuse counselors, psychiatric nurse practitioners, and psychiatrists. Interns are assigned to teams of psychiatrists, psychiatric nurse practitioners, and therapists for weekly case discussions and clinical presentations. This track allows interns opportunities to provide consultation on behavioral health leadership projects and complete inpatient consultations and evaluations on an as needed basis. Lastly, interns are provided with leadership opportunities including presentations at staff meetings, best-practice presentations, practicum student supervision, and participation in program development and behavioral health research projects.
The RRH Child/Adolescent track will provide trainees with experience and training providing behavioral health services to children, adolescents, and young adults. Interns are placed at Genesee Mental Health Child and Youth Clinic, an outpatient mental health clinic providing diagnostic and treatment services to individuals ages 5-18. The clinic includes a multidisciplinary team of licensed social workers, licensed mental health counselors, psychiatric nurse practitioners, and psychiatrists. Interns placed at this site are integrated into the multidisciplinary team and work with the team to address individual mental health needs and improve family functioning. Interns attend weekly team meetings and clinical rounds. Interns carry a caseload of individual clients and have the opportunity to conduct both individual therapy and family therapy. Interns are provided with training and opportunities to implement the following evidence-based treatments with children, adolescents, and their families; CBT, DBT, MI, ACT, and trauma-informed practices. The psychiatric characteristics of clients treated includes the full diagnostic range of the DSM-5 and clients presenting to the clinic represent a diverse patient population with respect to age, race, ethnicity, sex, and gender. In addition to therapy work, interns will also engage in psychological assessment in order to provide differential diagnoses and recommendations for ongoing treatment/referrals. Interns will learn efficient evaluation and report writing procedures. Additionally, if aligned with intern goals, interns are provided opportunities to provide consultation to school-based teams, chemical dependency teams, and adult mental health settings. Lastly, interns are provided with leadership opportunities including presentations at staff meetings, best-practice presentations, practicum student supervision, and participation in program development and behavioral health research projects.
The Neuropsychology Track places interns in the Neuroscience Institute in the Rochester Regional Health system. Neuropsychology interns are supervised by Clinical Neuropsychologists (four with board certification, and one in progress). This program is designed for students planning to become Clinical Neuropsychologists.
In outpatient and inpatient settings, interns conduct evaluations with people with a wide variety of neurological conditions. These can include ischemic stroke, cerebral hemorrhage, concussion, traumatic brain injuries, anoxic brain injury, brain tumor, metabolic and other encephalopathies, neurodegenerative disease/dementias, prolonged cognitive symptoms after COVID, and autoimmune neurologic disorders (such as multiple sclerosis). Additional typical presenting conditions include non-neurologically based conditions that cause cognitive dysfunction (such as Functional Neurological Disorder and depression) and substance dependence. The patient population is primarily adult and older adult, with limited opportunities to work with children and adolescents. At the Golisano Restorative Neurology & Rehabilitation Center at Unity Hospital there is a wide range of presenting conditions. This inpatient rotation provides the intern with training in efficient evaluation and report writing procedures, as well as hones brief psychotherapy skills. Within this program, interns also have opportunities to provide psychotherapy to patients with non-neurological conditions, such as orthopedic injuries or limb loss. Inter-disciplinary collaboration and presentations at staff conferences are regular components of the intern’s inpatient rehabilitation experience.
In the outpatient setting, the Intern participates in various outpatient clinics, as well as conducts neuropsychological evaluations with general outpatients. The Memory Center at Unity is a large component of the training experience. Within this clinic, interns learn to conduct evaluations with adult and older adult patients to assist with differential diagnosis. A large portion of these referrals pertain to diagnosis of dementia subtypes, including typical and atypical variants of Alzheimer’s disease, frontotemporal lobar degeneration, Lewy body disease, and patients with predominate cerebrovascular presentations. Interns will be involved in case consensus meetings with our neurology partners, which will include the opportunity to learn about advanced neuro-imagery (MRI and FDG/PET). The Concussion Clinic exposes the Intern to the complexities of post-concussion symptoms, including the psychological factors that may prolong and exacerbate symptoms. General outpatient referrals provide a context for training in comprehensive neuropsychological evaluation and report writing with a wide range of neurological patient populations. Here, there may be limited opportunities to provide psycho-therapy with neurological patients.
Interns participate in the inpatient program (25% of time) and all major outpatient clinics (75% of time). In addition, they participate in community education programs (including support and psychoeducational groups) and monthly Neuropsychology-specific didactics and case conferences. There are also monthly Neurology rounds within the department, as well as monthly Neuroradiology rounds with neurology, neurosurgery, and radiology providers.
The RRH Integrated Care clinical rotation provides trainees with opportunities to engage in the integrated care model of treatment, providing outpatient mental health services to individuals within their primary care, family care, and/or specialty care offices. Our offices are currently embedded within eight different practices in the greater Rochester Area. The embedded setting allows for thorough collaboration with the medical care team of each individual served, providing comprehensive care. The population served is diverse with the opportunity to gain experience in working with our refugee community, individuals struggling with chronic pain, as well as individuals with comorbidities. Interns will have the opportunity to engage in individual therapy, family therapy, and group therapy while also conducting comprehensive evaluations and psychological assessments. Interns will work on a multi-disciplinary team consisting of licensed social workers, licensed mental health counselors, and a psychiatrist, as well as with the medical team and physicians at their sites.
Rochester Psychological Assessment and Testing (RPAT) was founded to provide additional psychological assessment services to the greater Rochester, New York area. Located to the east between city and suburbs, RPAT is fifteen minutes from the RIT campus. RPAT internship track offers the unique opportunity to gain experience working within a busy, multidisciplinary private practice. Interns will receive supervision from RPAT’s team of licensed psychologists who draw from a wide range of training and practice backgrounds. The RPAT clinical assessment track provides trainees with opportunities to further develop skills in the primary areas of psychological evaluation and therapeutic intervention. At RPAT, interns conduct psychological assessment and evidence-based treatment in an outpatient office setting. In addition, the internship track provides an opportunity to learn about business practices and considerations when pursuing independent practice. Furthermore, Interns will have the opportunity to work with both children and adults and may consult with the RPAT team to emphasize either pediatric or adult practice, if desired.
Psychological assessment at RPAT includes evaluations for attention-deficit/hyperactivity disorder, autism spectrum disorder, comprehensive psychological evaluation, learning and cognitive functioning, dyslexia, court ordered evaluations, adaptive behavior assessments, sex offender risk assessments (if a desired experience), police officer candidate evaluations, pre-international adoption evaluations, and pre-surgical evaluations. RPAT provides services for the full diagnostic range of those in need of assessment or therapy; however, cases are driven by the individual needs of our clients. Most interns will also carry a small caseload of therapy clients. Additionally, interns consult and collaborate with referral sources that include primary care physicians and pediatricians, clinic and community therapists, psychiatrists and nurse practitioners, schools, and various community agencies. The goal of the RPAT internship track is to provide interns with lasting knowledge and experience working with a variety of cases and providing a range of services within an outpatient private practice setting.
For more information about our practice, visit: Rochesterpsychtesting.com
The Ontario County Mental Health (OCMH) Department is situated in the heart of Western New York, in the Finger Lakes Region. OCMHC’s Director of Community Services, Jessica Mitchell, Ph.D., through the Local Government Unit (LGU), is responsible for the distribution of funds (federal, state and/or local dollars), oversight and compliance of programs with State regulations, and the development of local plans for behavioral health services for individuals living with developmental, mental health, and/or substance or alcohol abuse disabilities in the community.
OCMH operates a certified outpatient mental health clinic treatment program, licensed by the New York State Office of Mental Health (OMH) through the Mental Health Department. The OCMH clinic serves individuals from ages 5 through adulthood, with a wide-range of psychological conditions or presenting concerns, from depression or anxiety, trauma or co-occurring disorders, to serious mental illness or emotional disturbances. The clinic offers evidence-based practice within the context of a multidisciplinary team approach, including psychiatric/medical providers, social workers, mental health counselors, peers/case workers, and in collaboration with other helping professionals or systems of care to support individuals’ recovery. Such as the Departments of Social Services, Public Health and Probation; as well as school districts, primary care offices, Health Homes case management providers, crisis service providers, local hospitals, etc. as needed or indicated.
OCMH’s internship training program includes a broad range of clinical and professional experiences within a rural, community-based setting, which can assist psychology interns in the development of their professional identity as providers of psychological services. Psychology interns would have opportunities to participate in didactic or training opportunities, as well as to develop, integrate, and synthesize their professional skills through a) direct clinical work (e.g., individual or group psychotherapy); b) consultation and involvement in county/community-based committees or programs (e.g., Ontario County Specialty Courts, Child or Adult Single Point of Access, Assisted Outpatient Treatment); and c) provision of psychological testing and evaluations for clients of the clinic and/or court-ordered evaluations (e.g., Family Court evaluations, “Persons In Need of Supervision” or PINS, Competency to Stand Trial).
One of the benefits of being a psychology intern (or licensed psychologist) in a rural or smaller community, within the LGU, as compared to a more urban or private agency/hospital, includes more regular or direct communication and partnerships with county and community partners such as attorneys, law enforcement, local leadership, etc. to further develop interns professional as well as leadership skills.
Psychology interns would also have opportunities to offer supervision to social worker or mental health counseling interns, offer in-service or educational trainings to clinical staff or other county/community partners, as well as opportunities to observe or participate in school-based clinic work or consultation groups depending upon interest.
Evidence-Based Practices
Interns will receive training in the following evidence-based practices: cognitive behavioral therapy (CBT), dialectical behavioral therapy (DBT), trauma-informed care, motivational interviewing (MI) and motivational enhancement therapy (MET) for addiction, relapse prevention, and integrated substance abuse and domestic violence (SADV) therapy. Training occurs through site-specific clinical trainings that occur at the beginning of the internship year, ongoing supervision by clinical supervisors, and a resource library for use by all trainees and staff.
Interns attend a weekly seminar series/didactics with clinical experts within the community. Interns will be able to observe and/or listen to presentations on diverse topics pertaining to current research on evidence based psychotherapy, assessment, consultation, trauma-informed practice, addiction research, ethics, professionalism, multiculturalism and diversity, interactive technologies, and telehealth as well as additional topics.
Research and Scholarship
All Interns are expected to conduct research at the internship sites through at least one ongoing “scholar project”, the focus of which is determined collaboratively between the primary supervisors and the intern. Interns are encouraged to focus their scholar project on substance use research and/or interactive technology. Interns are expected to develop rationale for their projects (i.e., a literature or evidence base), prepare a protocol for their projects (including submission to RIT IRB, if necessary), complete analyses of data related to their projects. Each internship site will orient interns to the amount of hours allocated to their scholar project.
Interns present their scholar project to their cohort, faculty, and community leaders at the end of internship. Interns also present their scholarly work at RIT’s Graduate Education Week and Showcase. Scholar projects can be:
- Independent projects unique to interns’ interests and career goals
- Unique approaches to existing work and projects at RIT clinical sites
- Reviews of intersections of digital and mechanical approaches to mental health
Scholar projects cannot be:
- The same project as intern dissertations
In addition to presentations, interns are encouraged to attend and submit to presentations at internal, regional, national, and international conferences. Interns are also encouraged to submit their scholarly work to publication. Should interns choose to submit their work to conferences or publications, there is support available to assist with this process.
Research Support
The RIT internship program includes multiple opportunities for scholarly support, which are incorporated into the curriculum. Interns will be assisted with their scholar projects by onsite supervisors and may attend research supervision meetings. Orientation to digital technology and mental health (e.g., eHealth) and supportive staff at RIT occurs throughout didactics, as seminars taught by specialists in engineering, computer science, and other disciplines who work in multidisciplinary digital mental health projects. Interns are supported in their interest to work or consult with any of these professionals.
View the 2022 Virtual Presentations
Graduate Show Case | RIT
2020 Winner in the Substance Abuse poster presentation category:
Examining Perceptions of Therapeutic Alliance and Treatment Outcomes in a Sample of Substance Using Offenders of IPV
https://vimeo.com/471535602
2020 Winner in the Psychology, Relationships, and Mental Health II poster presentation category:
Psychosocial consequences of COVID-19 among college students
https://vimeo.com/471097048
Interns may work with RIT faculty on substance use and violence research as well as research focusing on incorporating advancements in technology within clinical care. Intern may be involved in grant funded clinical research focused on the development of efficacious treatments for addiction, trauma, and violence including psychotherapy treatment trials. Interns have the opportunity to attend research seminars, meetings, and writing scholarly projects with faculty associated with addiction-focused NIH-funded or foundation funded research located within CHST’s School of Behavioral Health. Visit our website Forensic, Addiction and Violence Research with Interactive Technologies.



Local, National and International Research and Scholarship
- Telepsychology Resources Growing in Upstate New York
- An Innovative Approach to Helping the Homeless
- RIT Program Expands Access to Treatment for Homeless in Upstate New York
- RIT professor works to end domestic violence
- Psychologist revolutionizing addiction, aggression treatments
- Work with Economic and Social Research Council Seminar Series
- RIT Featured Faculty Scholarship
- Economic and Social Research Council Seminar Series speaker profile
- Economic and Social Research Council Seminar Series agenda
- Work by Assistant Professor Cory Crane
- Research in the College of Health Sciences and Technology (page 17)
- CT News Junkie: Study Recommends New Approach to Treating Family Violence Cases
- Report: Addressing Family Violence in Connecticut: Strategies, Tactics and Policies
- Study Briefing: Addressing Family Violence in Connecticut: Strategies, Tactics and Policies
Supervision
All interns receive at least 4 hours of supervision per week. Interns are provided two hours of individual supervision by a licensed psychologist who oversees the interns’ clinical work at their clinical sites. All interns participate in 1 hour of group supervision from RIT and 1 hour of additional group or individual supervision through their specific track or research.
Training Faculty
RIT
Interim Program Director, Research Faculty, RIT Behavioral Health and Forensic Psychology Programs
Deputy Intern Training Director, Supervisor and Research Faculty, RIT Behavioral Health and Forensic Psychology Programs
Hillside

Chris Dehon, PhD
Supervisor
Chris Dehon, PhD
Dr. Dehon is a licensed psychologist and internship supervisor working with Hillside Children’s Center. Dr. Dehon is the senior psychologist for Hillside Children's Center's residential program, where he has worked for the last 16 years. Dr Dehon works with children between the ages of 5 and 22 who have emotional and/or behavioral difficulties. He works closely with families in the treatment of their children.
Rochester Regional Health

Krista M. Damann, PhD
Supervisor
Krista M. Damann, PhD
Dr. Damann is a leader on the neuropsychology team. She diagnoses and treats the varied cognitive and psychological needs of patients with neurological conditions. She specializes in evaluating and treating patients with concussion, traumatic brain injury, stroke, and neurodegenerative disorders, such as Alzheimer’s disease. In addition to her general outpatient practice, Dr. Damann serves as a consultant to the Memory Center, the Concussion Clinic, and the inpatient brain injury unit at Golisano Restorative Neurology & Rehabilitation Center. Dr. Damann completed her Bachelor’s degree in Psychology at Roberts Wesleyan College in Rochester, where she also competed in intercollegiate basketball and was named an Academic All-American. She earned her Ph.D. in Counseling Psychology from the University at Albany, and completed a two year post-doctoral fellowship in neuropsychology at Comprehensive Neuropsychological Services in Albany, NY. She is board certified in clinical neuropsychology by the American Board of Professional Psychology (ABPP). Dr. Damann is an active member in numerous local and national neuropsychology organizations. She regularly conducts professional presentations on a number of topics, including brain injury, memory disorders, and emotional adjustment to neurological conditions. Dr. Damann enjoys supervising psychology graduate students, and she holds an appointment as a clinical instructor for medical residents at the University of Rochester in the Physical Medicine and Rehabilitation Department.

Tanya R. Grace, PsyD
Supervisor
Tanya R. Grace, PhD
Dr. Grace's approach to patient care is comprehensive and individualized. She gained an extensive history from her patients to be able to design an individualized assessment to their unique concerns/difficulties which allows her to provide the most appropriate neuropsychological diagnosis and treatment recommendations. Dr. Grace attended college at SUNY Oswego and obtained her Psy.D. in Clinical Psychology (with a specialization in neuropsychology) from Florida Institute of Technology in Melbourne, FL. Dr. Grace completed her neuropsychology internship at Emory University School of Medicine/Children's Healthcare of Atlanta, prior to a two-year post-doctoral fellowship in Clinical Neuropsychology at Florida Hospital/Walt Disney Pavilion in Orlando, FL. She returned to Rochester to bring her clinical skills and training to the Rochester area. She has extensive pediatric experience working in multiple neurodevelopmental, medical/neurological, and psychology settings with children as young as toddlers. Her love for working with older adults and the geriatric population stems from her many years of experience working at a state-funded memory center in Florida. She also provides clinical assessment and care to adults who are suffering from a range of neuropsychological concerns.

Melinda Ann Patterson, PsyD
Supervisor
Melinda Patterson, PsyD
Dr. Patterson is a Clinical neuropsychologist who specializes in clinical interviewing, clinical and forensic neuropsychological assessment, and development of treatment plans and intervention for a wide variety of brain-based disorders. Dr. Patterson works with individuals across the lifespan. She is an alumna of Georgetown University (2006) and earned her doctorate degree in Clinical-Community Psychology from the University of La Verne (2014). Her training emphasized a systems approach and an emphasis on prevention, as well as intervention, and she carries these perspectives in all of her clinical and supervisory work. After completing all of her pre- and post-doctoral training in Southern California, she worked in private practice in the Los Angeles area. Dr. Patterson joined Rochester Regional Health’s Neuroscience Institute in 2020. That year, she also joined the supervision team for the RIT Priority Behavioral Health internship. Dr. Patterson’s clinical specialties include developmental disabilities, learning disorders, concussion, and diagnoses related to aging, including dementias and stroke. She is passionate about supervising, mentoring, and teaching budding psychologists. She is also an adjunct Faculty Instructor at the University of Rochester.

William Schneider, PhD
Supervisor
William Schneider, PhD
Dr. Schneider provides oversight and vision for our expanding neuropsychology services. From a clinical perspective, he specializes in pediatric and adult neuropsychological assessment and brain injury rehabilitation. He works to promote optimal cognitive outcomes after brain injuries, focusing on behavioral management in rehabilitation. He also acts as a liaison and consults with schools and educational programs. He has conducted collaborative research over the years with his medical and neuropsychological colleagues on the topics of pharmacotherapy for enhancing cognitive outcome and functioning in traumatic brain injury. His extensive list of research and presentations include topics in cognitive and behavioral disorders and rehabilitation following traumatic brain injury. Dr. Schneider earned his B.A. in Psychology from Wheaton College and his PhD in Clinical Psychology, APA Accredited Program from the Biola University, Rosemead School of Psychology in La Mirada, California. His APA-accredited doctoral internship was completed at Pine Rest Christian Hospital in Grand Rapids, Michigan; his post-doctoral Fellowship in Rehabilitation and Neuropsychology was completed at the University of Michigan Medical Center in Ann Arbor. Dr. Schneider is actively involved in graduate psychology and medical education. He has maintained a clinical appointment at the University of Rochester Department of Physical Medicine and Rehabilitation for over 20 years, where he provides training, gives lectures and helps lead journal club for a group of medical residents in rehabilitation medicine. He has also been supervising graduate psychology students for over two decades as an agency supervisor for the State University of New York at Brockport Masters in Psychology Program.

Garry Spink, PhD
Supervisor
Garry Spink, PhD
Dr. Spink received his PhD in Clinical Psychology from Syracuse University. He completed his doctoral internship and post-doctoral fellowship with Rochester Institute of Technology and Rochester Regional Health. He joined Rochester Regional Health as a psychologist in July 2020. At this time, he serves as the primary site supervisor for interns placed at Rochester Regional Health Adult Outpatient clinics. Dr. Spink’s clinical focus falls in the broad category of Health Psychology and Behavioral Medicine; however, his overall focus is on assessment and treatment of people with chronic pain. Dr. Spink also has experience helping people with neurological conditions, fatigue, gastroenterological conditions, cardiovascular disease, sleep, and stress management. While Dr. Spink’s primary area of practice is in chronic pain and illness, he also consults and does work with personality disorders.
CCSI

Elizabeth Meeker, PsyD
Supervisor
Elizabeth Meeker, PsyD
Dr. Elizabeth Meeker, Senior Director, System and Practice Transformation at CCSI, leads a team of talented professionals who provide training, coaching, consultation and practical tools to make trauma-responsive practices a living, breathing part of systems, organizations and daily work. She is a seasoned consultant working with a broad range of healthcare and human service organizations to implement and integrate practice change initiatives to improve outcomes and sustain change. Dr. Meeker also serves on the CCSI Talent and Culture Team charged with developing strategies, resources, and professional development for all CCSI employees in the areas of talent management and learning; organizational wellness and trauma informed practices; corporate compliance and business ethics; diversity, equity, inclusion and anti-racist practices. In addition, she is a Qualified Teacher of Mindfulness Based Stress Reduction with a particular focus on enhancing staff wellness. She is a licensed clinical psychologist and has a private clinical practice specializing in children, adolescents and young adults. Dr. Meeker completed her doctoral internship training at Hutchings Psychiatric Center in Syracuse, NY and received her PsyD in Clinical Psychology from Indiana State University, a MS in Psychology from Indiana State University, and a Bachelor of Arts in Psychology from Wellesley College.
University of Rochester Medical Center (URMC) Strong Recovery

Cassandra Berbary, PhD
Internship Training Director

Cory Crane, PhD
Supervisor

Caroline Easton, PhD
Supervisor
Rochester Psychological Assessment & Testing (RPAT)

Brian Amos, PhD
Supervisor

Nicole Giboson, PhD
Supervisor

Jake Swartwout, PsyD
Supervisor

Kristy Kelley, PsyD
Supervisor
Ontario County Mental Health (OCMH)

Jessica Mitchell, PhD
Supervisor
Additional Training Faculty

Latrease Moore, PhD
Supervisor

Rebecca Zill, PsyD
Supervisor
Didactic Seminar Series
Interns receive 2 hours of didactic training each week. Didactic training is incorporated to further support interns’ continued growth and development. Didactic training includes training provided by RIT faculty, consortium supervisors, and experts and professionals from the community. Didactic training focuses on the training program competencies and includes topics such as; multiculturalism and diversity; professionalism; evidence-based therapy; assessment and report writing; trauma-informed care; self-care and vicarious trauma; substance use prevention, intervention, recovery, and research; forensic psychology; consultation; program evaluation; ethics; interactive technology; additional special topics.
Stipend, Benefits, and Resources
Stipends are provided in the amount of $36,500. Interns are classified as independent contractors, will receive a 1099 form, and are responsible for paying taxes on their stipend. Interns are eligible to enroll in student health coverage. Interns will be provided with office space, computers, and access to IT and administrative support.
Application Process and Selection Criteria
Students interested in applying for the internship program should submit an online application through the APPIC website (www.appic.org).
Application due date: December 1st
A complete application consists of the following materials, which are all part of the online AAPI:
- Completed Online AAPI
- Cover letter
- Current Curriculum Vitae
- Three Standardized Reference Forms, two of which must be from persons who have directly supervised your clinical work. Please submit no more than three letters
- Official transcripts of all graduate coursework
- Supplementary materials: One full integrated assessment report (please redact appropriately)
*All samples must be de-identified, removing all identifying client information. Breaches of confidentiality within submitted samples will disqualify your application for further consideration and your program’s Director of Clinical Training will be notified.
All application materials must be received by the APPIC deadline in order to be considered. Applicants who are invited to interview will be notified by email. Interviews will be scheduled in January/February and will occur either in person or via videoconference. Phone interviews will be provided in cases where videoconference is not an option.
The program bases its selection process on the entire application package noted above; however, applicants who have met the following qualifications prior to beginning internship are considered preferred:
- Preferred. Minimum of 400 intervention hours (experience with CBT, MET, DBT, Trauma-Focused Interventions)
- Preferred. Minimum of 200 assessment hours (experience administering cognitive, neuropsychological, personality measures with experience in integrative Report Writing)
- Preferred. Dissertation proposal defended or data collected/ date set.
- Interest in Telehealth and Interactive Technologies
- Some experience or special interest in working with diverse populations
In addition to the above consortium-wide preferences, RIT will consider specific aspects of the applicant’s experience, interests, and training goals in determining an applicant’s potential “fit” with individual clinical training sites. Applicants are encouraged to carefully review the descriptions of the training sites and to highlight areas of perceived fit within their cover letters.
In general, the internship program prefers that interns have completed intervention hours that include experience with CBT, MET, DBT, and/or Trauma Focused interventions. In terms of assessment experience, the program looks for experience administering such measures as the WISC, WAIS, WMS, MMPI, and the PAI as well as experience with integrated report writing.
Each site also has its own preferences for practicum experiences which are as follows:
- CCSI looks for applicants who have research experience and proficiency in conducting clinical research and consultation.
- Hillside prefers applicants who have practicum experience with children and adolescents and youth exposed to trauma.
- RIT Priority Clinic prefers applicants with outpatient practicum experiences.
- Rochester Regional Health (RRH) Outpatient Behavioral Health (Adult) Track also prefers applicants with prior outpatient practicum experiences.
- Rochester Regional Health (RRH) Outpatient Behavioral Health (Child/Adolescent) Track seeks applicants with outpatient and/or school-based therapy experience.
- Rochester Regional Health (RRH) Neuropsychology at the Neuroscience Institute Track requires applicants have previous practicum experience in neuropsychology.
All interns who match must successfully pass a background check conducted by RIT, as well as obtain a TB test, before beginning employment. Clinical sites may require site specific clearances, background checks, and/or drug testing. All interns are required to abide by COVID-19 policies set by RIT and their specific training sites, which currently includes COVID-19 vaccination and compliance with required personal protective equipment. Applicants are advised that the internship requires regular travel between training sites, and thus Interns must have consistent access to reliable transportation.
This internship site agrees to abide by the APPIC policy that no person at this training facility will solicit, accept, or use any ranking-related information from any intern applicant.
Questions regarding the selection process may be directed to the Internship Training Director, Dr. Cassandra Berbary at cmbihst@rit.edu.
Internship Handbook
For additional information regarding the internship program, please see the internship handbook.
Intern Expectations
With regard to intern behavior and performance during the training year, the general expectations of RIT’s internship program are that the intern will:
- Adhere to the APA Ethical Principles of Psychologists and Code of Conduct
- Operate within the bounds of the laws and regulations of the New York state
- Adhere to the policies and procedures of Rochester Institute of Technology
- Adhere to the policies and procedures of intern’s assigned tracks
Formal evaluations are completed 3 times a year, during the year and serve as a review of progress on training goals and core competencies. To progress in the program and to successfully complete the program, Interns must demonstrate minimum levels of achievement across all required elements. Evaluations are conducted using a standard rating form, which includes comment spaces where supervisors include specific written feedback regarding the Interns’ performance and progress. Supervisors will review these evaluations with the Interns and provide an opportunity for discussion if the Intern has questions or concerns about the feedback. Copies of all evaluations are found in the internship handbook linked on this website.
A minimum level of achievement at the 1st and 2nd evaluation time points are defined as a rating of “3” (Intermediate Competence) for each element. The rating scale for each evaluation is a 5-point Likert scale. If an Intern receives a score less than 3 on any element, or if supervisors have reason to be concerned about the Intern’s performance or progress, the program’s Due Process procedures will be initiated. The Due Process guidelines can be found in the internship handbook. A minimum level of achievement at the 3rd evaluation time point (end of the training year) is defined as a rating of “4” (Proficient Competence) for each element. Meeting the minimum level of achievement at the end of the year includes having; 1) the ability to independently function in a broad range of clinical and professional activities; 2) the ability to generalize skills and knowledge to new situations; 3) the ability to self-assess when to seek additional training, supervision or consultation.
Additionally, Interns are expected to complete 2000 hours of training during the internship year. Meeting the hours requirement and obtaining minimum levels of achievement on evaluations demonstrates that the Intern has progressed satisfactorily through and completed the internship program. Evaluations will be maintained by the Training Director and will be accessible to the Intern for future review if requested. Feedback to the Interns’ home doctoral program is provided at the 2nd evaluation time point and at the culmination of the internship year. Doctoral programs are contacted within one month following the end of the internship year and informed that the Intern has successfully completed the program.
If successful completion of the program comes into question at any point during the internship year, or if an Intern enters into the formal review step of the due process procedures due to a grievance by a supervisor or an inadequate rating on an evaluation, the home doctoral program will also be contacted. This contact is intended to ensure that the home doctoral program is kept engaged in order to support an intern who may be having difficulties during the internship year. The home doctoral program is notified of any further action that may be taken by the internship program as a result of the due process procedures, up to and including termination from the Program. See the Due Process procedures outlined in the internship handbook for more information about the process of and conditions for termination.
HRSA Grant Funding
According to federal funding regulations, HRSA funded intern applicants are subject to additional eligibility criteria per Funding Opportunity Announcement (NOFO), HRSA19002. Intern applicants for the HRSA funded positions must be in an APA accredited program, a citizen of the United States, a non-citizen national of the United States, or a foreign national who possesses a visa permitting permanent residence in the United States. Individuals on a temporary or student visa are not eligible for HRSA funded internship slots. Applicants will be required to verify their compliance with this citizen/visa status prior to award of any federal funding.
Training Clinical Psychology Interns to use Evidence-Based Care Models and Tele-Behavioral Health Technology to Treat OUD and SUD in Monroe County
The internship proposes to increase the number of doctoral psychology interns trained to provide culturally-competent, interdisciplinary behavioral health and substance use services for the highly underserved communities of Monroe County in upstate New York. Monroe County is a rural area facing considerable behavioral health workforce challenges. The internship program is a key resource in the area both for providing behavioral healthcare to underserved citizens as well as providing high-quality interdisciplinary training.
The program aims to improve the doctoral psychology internship program’s capacity to train psychology interns in behavioral health and substance use prevention and treatment. Specifically, funding will be used to train 21 additional interns during the grant period, with 7 internship slots added in each grant year. Grant funding will allow for enhancement of the current interdisciplinary training in Opioid Use Disorder (OUD) and other Substance Use Disorder (SUD), as well as the increased provision of training in tele-behavioral health. The specific, measurable objectives associated with the proposed project are as follows: 1) Between September 2019 and August 2022, add a total of 21 intern training positions with a focus on OUD/SUD services for underserved populations; 2) Between September 2019 and August 2022, the program’s existing integrated care training curriculum will be enhanced through the addition of new annual training activities and rotations; 3) By August 2022, the program will have improved its training of psychology interns in OUD/SUD through faculty development; 4) By August 2022, the local healthcare workforce will be expanded and enhanced through the retention of at least 60% of trainees. All project activities have been developed with an emphasis on training interns to provide culturally competent care for vulnerable, diverse, and underserved populations
This program is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under D40HP33360 and Graduate Psychology Education Programs as part of an award (Training Clinical Psychology Interns to use Evidence-Based Care Models and Tele-Behavioral Health Technology to Treat OUD and SUD in Monroe County) totaling $1,341,194 with 0% non-governmental sources. The information provided on this website is that of the internship program and director and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
Expanding Evidence-Based Mental Health and Integration of Care Models among Children and Adolescents in Upstate New York via an Accredited Doctoral Psychology Internship Training Program
The internship aims to increase training opportunities and the number of doctoral psychology interns trained to provide culturally-competent, interdisciplinary behavioral health services for children, adolescents, and transitional youth in highly underserved communities of Monroe County in upstate New York. Monroe County is facing considerable behavioral health workforce challenges. The internship program is a key resource in the area both for providing behavioral healthcare to underserved citizens as well as providing high-quality interdisciplinary training.
This project will improve the clinical psychology internship program’s capacity to train psychology interns in integrated behavioral health and primary care settings with a focus on the treatment of children, adolescents, and transitional age youth. Specifically, funding will be used to train 32 additional interns during the grant period, with 6 internship slots in year 1, 6 internship slots in year 2, 10 internship slots in year 3, and 10 internship slots in year 4. Grant funding allows for enhancement of integrated care training as well as the increased provision of training in 1) utilizing advancements in technology within integrated treatment; 2) addressing co-occurring disorders (OUD/SUD and mental health) among youth, and 3) prevention and treatment related to violence exposure among youth. The specific, measurable objectives associated with the proposed project are as follows: 1) Between July 2021 and June 2025, add a total of 32 intern training positions with a focus on providing behavioral health services to children, adolescents, and transitional youth in integrated care settings; 2) Between July 2021 and June 2025, the program’s existing integrated care training curriculum will be enhanced through the addition of new annual training activities and rotations; 3) Between July 2021 and June 2025 the program will have improved its training of psychology interns in integrated care through faculty development; 4) By June 2025, the local healthcare workforce will be expanded and enhanced through the retention of at least 50% of trainees. All project activities have been developed with an emphasis on training interns to provide culturally competent care for vulnerable, diverse, and underserved children, adolescents, and transitional age youth.
This project is supported by the Health Resources and Services Administration (HRSA-21-089) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $1,510,162 with 0% financed with non-governmental sources. The information provided on this website is that of the internship program and director and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
Internship Admissions, Support, and Initial Placement Data
Date Program Tables updated: July 1, 2025
Program Disclosures
| Does the program or institution require students, trainees, and/or staff (faculty) to comply with specific policies or practices related to the institution’s affiliation or purpose? Such policies or practices may include, but are not limited to, admissions, hiring, retention policies, and/or requirements for completion that express mission and values? | ___ Yes _X_ No |
Internship Program Admissions
| Briefly describe in narrative form important information to assist potential applicants in assessing their likely fit with your program. This description must be consistent with the program’s policies on intern selection and practicum and academic preparation requirements: |
| In general, the internship program prefers that interns have completed intervention hours that include experience with CBT, MET, DBT, and/or Trauma Focused interventions. In terms of assessment experience, the program looks for experience administering such measures as the WISC, WAIS, WMS, MMPI, and the PAI as well as experience with integrated report writing. Additionally, the internship program prefers individuals who 1) have their dissertation data collected or have defended their dissertation, 2) have an interest in telehealth and interactive technologies, and 3) have some experience or special interest in working with diverse populations. |
| Does the program require that applicants have received a minimum number of hours of the following at time of application? If Yes, indicate how many: | |||
| Total Direct Contact Intervention Hours | Amount: 200 hours | ||
| Total Direct Contact Assessment Hours | Amount: 400 hours | ||
Financial and Other Benefit Support for Upcoming Training Year*
| Annual Stipend/Salary for Full-time Interns | $36,500 | |
| Annual Stipend/Salary for Half-time Interns | NA | |
| Program provides access to medical insurance for intern? | Yes | No |
| If access to medical insurance is provided: | ||
| Trainee contribution to cost required? | Yes | No |
| Coverage of family member(s) available? | Yes | No |
| Coverage of legally married partner available? | Yes | No |
| Coverage of domestic partner available? | Yes | No |
| Hours of Annual Paid Personal Time Off (PTO and/or Vacation) | 3 weeks | |
| Hours of Annual Paid Sick Leave | 5 days | |
| In the event of medical conditions and/or family needs that require extended leave, does the program allow reasonable unpaid leave to interns/residents in excess of personal time off and sick leave? | Yes | No |
|
Other Benefits (please describe): Interns are provided with laptops, office space, and access to IT and administrative support. |
||
*Note: Programs are not required by the Commission on Accreditation to provide all benefits listed in this table.
Initial Post-Internship Positions
(Provide an Aggregated Tally for the Preceding 3 Cohorts)
| 2021-2024 | ||
| Total # of interns who were in the 3 cohorts | 58 | |
| Total # of interns who did not seek employment because they returned to their doctoral program/are completing doctoral degree | 1 | |
| PD | EP | |
| Academic teaching | 5 | 0 |
| Community mental health center | 4 | 0 |
| Consortium | 0 | 0 |
| University Counseling Center | 2 | 0 |
| Hospital/Medical Center | 16 | 0 |
| Veterans Affairs Health Care System | 2 | 0 |
| Psychiatric facility | 0 | 0 |
| Correctional facility | 0 | 0 |
| Health maintenance organization | 0 | 0 |
| School district/system | 0 | 2 |
| Independent practice setting | 17 | 2 |
| Other | 5 | 2 |
Note: “PD” = Post-doctoral residency position; “EP” = Employed Position. Each individual represented in this table should be counted only one time. For former trainees working in more than one setting, select the setting that represents their primary position.
Past Intern Cohorts
2019-2020 Cohort
Top left to right: Taylor Dreste, Jacob Wadsworth, Jonathan ‘Tory’ Toole
Bottom left to right: Alesia Allen, Courtney Chappell, Anna Pignatiello, Rupa Kalahasthi
2020-2021 Cohort
Top left to right: Melissa Morton, Kayla Kleinman, Alexis Liberto, Martha Golubski,
Alessandra Perez, Jenna Steinmiller, Kane Williams, Justin Gardner, John Mansoor
Bottom left to right: Stephanie Rovig, Mary Moussa Rogers, Celeste Sangiorgio

2021-2022 Cohort
From Left to Right: Tim Baer, Eljada Gjoka, Dustin Haraden, Noora Abdulkerim,
Jaime Blackmon, Constance Rose, Thomas Chacko, Leah Ward, Siena Tugendrajch,
Johnathan Wright, Joanne Raptis, Kayci Hauser

From Left to Right: Mini Mathai, Kalpana Sundaram, Marielsy Pimentel, Kristy Kelley,
Deon Allen, Qian Li

2022-2023 Cohort
Left to right (front): Pooja Melkote, Alexis Rhames, Taylor Steeves, Taylor Clark, Brittany Pereira
Heather Guercio, Natalie Nordlund
Left to right (back): Ellen Masters, Emily Helminen, Courtney McKinney, Kirstie Pysher,
Jourdan Rodak, Alexey Breuss, Megan Scroger, Ryan Peleaux, Michael Huddleson

2023-2043 Cohort
Left to right (front): Lauren Monthie, Sally Kafelghazal, Jana Elrabaa, Thao Nguyen, Coral Jimenez-Ricaurte,
Lilybeth Valencia, Yasmin Arias, Heather Darby, JorDaSha Atchison, Camela Barker, Kait McElroy
Left to right (back): Frank Robertson, Valerie Sclesa, Sydney Brown, Victoria Pezzino, Danielle Pendarvis,
Kay Darling, Gretchen Landry, Douglas Welsh, Andrew Lambiase, Alex Bonagura
Not pictured: Javier Marthillo, Moriah Splonkowski

2024-2025 Cohort
Left to right (front): Veronica Altamirano, Alexandra Maldonado-Santiago, Michelle Jeon, Maya Hareli,
Eva Tetteyfio, Sarah Carroll, Megan Fok, Sydney Hernandez, Henna Dhingra
Left to right (middle): Casey Ameda, Sam Loomis, Nicholas Semaan, Andrea Gottfried, Taylor Achtyl,
Sabrina Gambino
Left to right (back): Gianna Rinaldi, Megan Zommers, Samantha Maguire, Hasad Freitag, Anna Miles,
Cheyenne Grice