Telehealth connects homeless with therapists training at RIT
A. Sue Weisler
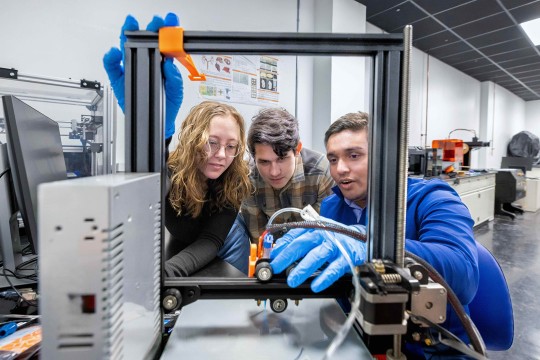
In a picture taken prior to the coronavirus pandemic, intern Jacob Wadsworth, left, prepares for an intake session with a House of Mercy guest. Caroline Easton, supervising psychologist, explains how to interface with the technology for remote therapy sessions.
Residents of a homeless shelter in Rochester are continuing to receive therapy during the coronavirus pandemic from a team of therapists in a clinical internship program at Rochester Institute of Technology.
The doctoral training program began as an exercise in using telepsychology to deliver care to a marginalized and underserved population. When New York shut down in March to stem the spreading virus, the therapists were already prepared to apply the telehealth protocols in the crisis.
“We didn’t skip a beat because we had this going pre-COVID-19,” said Caroline Easton ’90 (biotechnology), professor in the biomedical sciences program. “We had already started implementing our telepsych program at the House of Mercy homeless shelter. We’re able to talk to them on the phone and give them emotional support and ease their anxieties and help with cravings.”
A. Sue Weisler
RIT professor Caroline Easton started a program to offer therapy to homeless clients at the House of Mercy. She is training therapists to conduct therapy in person and via remote technology. “Without treatment, things can really spiral out of control,” Easton said. “We work with people to help stabilize and get support services in place.”
Easton, who is also director of RIT’s Priority Behavioral Health and Clinical Psychology Internship, funded the training program at House of Mercy with a $1.4 million grant she received from the U.S. Department of Health and Human Services. The grant helped purchase the teleconferencing technology—video cameras, monitors, tablets—and make the program possible in conjunction with support Easton and the House of Mercy won from Greater Rochester Health Foundation, Max and Marian Farash Charitable Foundation, and ESL Charitable Foundation.
“Caroline and her team are reaching out personally to those within the house who are mentally ill and checking in with them,” said Sister Grace Miller, founder and executive director of House of Mercy. “Right now, Caroline is our only support for our folks.”
Thousands of homeless people in the Rochester community rely on at the House of Mercy for food, shelter, counseling and advocacy. Sister Grace and her small staff are watching the residents closely. They installed washing stations and are taking temperatures daily.
A. Sue Weisler
Psychology intern Rupa Kalahasthi, left, talks to Sister Grace Miller, right, about the therapy services. Miller, executive director, opened House of Mercy in 1985.
“We’ve put some of our guests at a hotel, directed by the county, and kept some here,” she said. “We have a real concern for the lack of care for the mentally ill. They’re not getting the help they need, especially now during this crisis. They’ve been forgotten.”
Many of the homeless residents are in poor health and suffer from diabetes, compromised immune systems, hypertension, cardiac issues and liver-related problems from years of substance, Easton said. Mental illness and substance use and addiction are prevalent as well. Without easy access to services, homeless people either never get behavioral health treatment or rely on costly emergency room services to meet their needs.
“Homeless people deserve best practices as well,” Easton said. “Why not bring treatment to them instead of setting them up for failure by asking them to go to a social services agency they can’t make it to or that turns them away when they arrive? Now, with COVID, it’s different for everyone. It’s all telepsych.”
All seven interns in Easton’s program this year have gained experience counseling homeless clients, either one-to-one via telehealth or in-person at the shelter. Under Easton’s supervision, they have learned to stabilize any psychiatric distress their clients present by using harm reduction and crisis management techniques. When the teleconferencing equipment arrived in January, they began to connect remotely from RIT’s onsite clinic to a private room at the House of Mercy, using telehealth protocols outlined by the American Psychology Association.
“The client sat in a seat facing a screen where they saw us also sitting in a therapy chair in one of our clinic rooms at our RIT internship site,” Easton explained. “We were able to talk to them as if they were right across the room from us.”
The new reality
When the soaring COVID-19 death rate forced the state’s closure, Easton let the shelter use the equipment for residents’ needing telemedical care. She regrouped with her team and adopted the state’s expanded telehealth guidelines for psychological care during the crisis.
The therapy interns were ready to help their clients but first they had to find them. Disconnected phone numbers or general lines to the House of Mercy’s front desk or to the hotel where some residents were relocated to reduce the shelter’s number made it difficult to track them down, said Jacob Wadsworth, an intern from Pittsburgh, Pa.
“How do you stay in place when you don’t have a place?” Wadsworth asked. “First and foremost, it’s making sure that they’re safe. That they have food, water, shelter—those basic needs are being met and making sure they are OK. Once we can make sure they have that kind of stability, then we can work on coping skills.”
Normally, the interns would meet new clients for the first time in person as part of the intake process, but in these circumstances, the interns began offering emotional support to any shelter resident in need via cell phone or over a Google line between the hotel and shelter that Easton initiated.
“This individual one-on-one is extremely important to them,” Sister Grace said. “They need someone to talk to, but they won’t tell their stories unless they’re comfortable. You must win their trust. Once they have your trust they will open up and you will really know what they are going through.”
Recently the therapy team has returned to the shelter for Thursday morning sessions with clients who have requested mental health services. Easton and three interns, wearing gloves and 3D printed masks—including some made by Sean Bellefeuille ’20 (bioengineering), CEO at M3Dimensions—enter the shelter after a temperature check. They disinfect their workspace and equipment, and start meeting individual clients to assess their concerns. The onsite team escorts the client to a private room where another intern, working remotely, leads the televideo session from their home office.
“We’ve also started going to the hotel where the other half of the House of Mercy clients are staying,” Easton said. “We set up our telehealth cart in a confidential room off the lobby. It's all new now. We have to adapt to the changing environments and symptoms that COVID has brought us.”
The Priority Psychology Internship Program
The Priority Psychology Internship Program is one of the few programs in the area to offer telehealth training to Ph.D. interns seeking required clinical experience, Easton said. Supervising physicians at Rochester General Hospital collaborate with Easton’s group through a partnership created by the RIT & Rochester Regional Health Alliance.
Easton developed the competitive one-year program that follows her individualized treatment method for helping people with substance use/addiction, aggression, and partner/family violence as interrelated issues.
“This year’s internship group has been the foundation of our telepsych program,” Easton said. “We’ve built this together, from the ground up, creating an infrastructure and confidential space and looking at the homeless guests as our partners. That the interns were able to switch gears and continue to help our clients during the lockdown shows how committed they are to quality care and how relevant this program is in Rochester.”
After the internship concludes in late June, Wadsworth will join Easton’s team as a postdoctoral researcher working with adolescents. Wadsworth’s experience with homeless clients has resonated with him. “From the first intake, I got the sense that we were doing was needed and important. I could watch the distress level decrease the longer they spent with us.”
Easton and her team collect data assessing clients’ stress level from zero to 10 before and after therapy, and the results are promising. The data shows clients’ feelings of extreme distress dropped from 76 percent to 41 percent directly before and after the initial intake session.
“We’re seeing differences in distress levels so that we know that something is happening. It’s working, Easton said.”
The coronavirus has expedited the need for telepsychology service. For Easton, the crisis has validated her decision to expand the internship to include remote therapy. The crisis has also influenced how the program will look for the 12 interns starting in July.
“We are adapting content and developing a training program that can function remotely to all telehealth and digital platforms so that we can continue providing quality care and training,” Easton said. “Even if we don’t need to, we’re still going to do it because it’s comprehensive, efficient and data driven.”
About Caroline Easton
Caroline Easton developed the Substance Abuse-Domestic Violence Behavioral Model to focus on reducing substance use in her clients while teaching them healthy coping skills for handling negative emotions. The client-centered approach is grounded in cognitive behavior theory and has measurable outcomes.
Easton conducted randomized control trials in 2006–2010 and 1998-1999, funded by the Donaghue Foundation and the National Institute of Drug Abuse. Easton’s work connects the dots between intimate partner/domestic violence, mental health, and substance abuse.
Clinical psychologists in the United Kingdom and in Australia use Easton’s method as an alternative therapy to court-referred programs that treat anger management, mental health, and/or substance abuse as unrelated issues.
Internship
The accredited Priority Psychology Internship Program in RIT’s College of Health Sciences and Technology offers clinical and research experience for doctoral students in clinical psychology. Interns learn to administer Easton’s integrated approach to treating co-occurring addiction/substance abuse and domestic violence among male offenders.
Interns gain experience administering addiction treatment at Rochester Regional Health and Hillside Children’s Home, and consulting and program evaluation at Coordinated Care Services Inc.
“I believe we are doing some very innovative work, and our goal is to recruit interns from across the United States to train in this area through our clinical psychology internship program,” RIT professor Caroline Easton said. “We have increased our training slots because we want to draw in the best intern candidates to recruit to upstate New York.”